
Simon Marks 4pm - 7pm
8 September 2020, 14:16 | Updated: 16 November 2020, 19:23

It was just over a week before the UK went into lockdown that Amy Durant developed a fever, body aches, tiredness, headaches, a cough - all symptoms of the novel coronavirus.
Now, nearly seven months later, the 31-year-old still hasn't recovered, and says the illness' immediate symptoms have since evolved into others.
"It has changed my life completely," Ms Durant told LBC on Tuesday. "I can’t exercise. Occasionally I leave the house because I am desperate to go for a walk but it usually results in the next few days being bedridden.
"I can’t work a lot of the time."
READ MORE: Long covid sufferers 'have symptoms for more than three months'

Hancock: NHS will have 40 'long-Covid' centres in place by end of month
Ms Durant, who co-owns London publishing company Sapere Books, described her experience as one where her initial symptoms cleared up after the first ten days, but by the end of the fortnight she had relapsed.
She said: "I started getting chest pain and breathing problems. Paramedics then came to assess me but my blood oxygen was fine so I stayed at home.
"After that I thought I was improving again and started going for runs.
"But then I got hit with debilitating fatigue to the point that I could barely leave the bed and persistent chest pain.
"That was in May, and it has been the same ever since."
READ MORE: Brits told to maintain COVID-19 safety rules after rise in cases

Ms Durant is not alone in experiencing this lengthy recovery process from COVID-19 that many of her fellow sufferers have called: "Long Covid".
In fact, the government reported on Monday that it believed around 10% of people who have experienced the virus without being admitted to hospital have then had symptoms for more than four weeks.
This recovery time, however, was doubled for those who have been treated in hospital.
Such symptoms include respiratory issues, fatigue, diarrhoea, headaches and skin rashes. Others, on social media, have also reported experiencing hair loss.
READ MORE: "We're blinded by the people we're not testing," says infectious disease expert
#LongCovid #CountLongCovid
— Dr Birgit Clark (@BirgitC) September 6, 2020
Another Sunday .... is this never going to end? Day 174. pic.twitter.com/JLCiBBHNZZ
Another fun symptom of #LongCovid hair loss, even with gentle brushing. #longhaulers # longhauler pic.twitter.com/AaGtYG6ovX
— Robbie McGillivray (@RobbieMcGilliv1) September 7, 2020
In an address to the Commons on Tuesday, Matt Hancock said there had also been a significant number of people experiencing symptoms for an even longer period.
The health secretary said that while there were 300,000 people who were still unwell after a month, there were around 60,000 people who were reporting issues for three months or more.
This was the case for Paul Garner, a professor at the Liverpool School of Tropical Medicine, who got sick in March and had several months of recurring illness that "floored" him.
READ MORE: GPs 'recorded three times more suspected cases of COVID-19 than official figures'
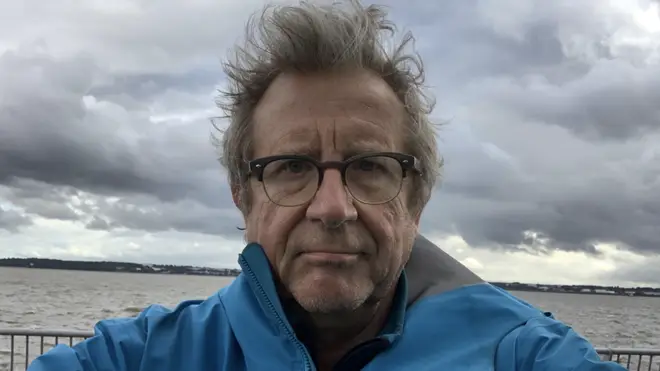
In the months that followed his initial recovery, he said he then experienced fatigue and other episodes that left him bedridden.
He told LBC: "I went for a cycle ride to my sisters birthday. It was only seven minutes there and seven minutes back.
"Because it pushed my heart rate up, I was in bed for three days after.
"A week ago, I realised that I won’t be better until - at the earliest - March next year, and may never be completely well again.
"The uncertainty does my head in."

28-year-old Long Covid sufferer warns young people of long term effect
Dr Rachel Pope, a senior lecturer in Archaeology, described to LBC the "onslaught" of her own symptoms after relapsing around five weeks into her recovery from the virus.
As a non-smoker and someone who only drinks socially, the 44-year-old said she was now dealing with high blood pressure, which had "never been a problem before".
"I couldn't walk for ten weeks," she said. "I have been sent to A&E three times with suspected heart attacks.
"There have been half a dozen times where I didn't think I would wake up. I've lost control of my bowels twice."
She added: "I'm quite a pragmatic person; I'm quite level-headed, but I have genuinely never experienced anything like this in my life.
"It has almost been worse than childbirth."
READ MORE: What is the new island quarantine policy? And how will it affect you?

While scientists are still early-on in the process of discovering everything there is to know about COVID-19, researchers in Glasgow have now launched a study examining long-term health impacts of the virus.
They are specifically looking into the prevalence and risk factors of long-term health and psychosocial consequences of the disease.
READ MORE: Holiday quarantine: Which countries are exempt and could future changes affect my booking?
For Prof Garner, who regularly writes for the British Medical Journal on the topic, he compared his "extremely similar" symptoms with that of chronic fatigue syndrome (ME/CFS).
He added: "No-one wants to go there because of the stigma. But the ME/CFS community have been really helpful and they have fantastic tools and things to help.
"Problem is that GPs in this country think ME is a psychological disease. Some people that have had CFS/ME and that now have Long Covid said this is different."
READ MORE: First Welsh local lockdown to be introduced in Caerphilly
Matt Hancock urges young people to take social distancing more seriously
There are currently tens of thousands of people joining Long Covid community groups online, where sufferers have been sharing their experiences of the illness.
According to Dr Pope, there are also three things for which they are advocating.
Aside from further research, she said: "Recognition and rehab - we need sufferers to not be pushed back into their workplaces if they're not ready.
"They may need a phased return or reasonable adjustments. We can't just rely on tests to be the factor; it needs to be symptom-based."