
Iain Dale 7pm - 10pm
7 January 2021, 11:51 | Updated: 7 January 2021, 11:55

NHS staff 'shattered' as pandemic's grip takes hold
NHS staff at a London hospital have said they are working "to the limit" of their ability in rare footage from a coronavirus ward.
Shattered healthcare workers at St George's Hospital in Tooting, south-west London, said they are battling low morale, exhausting shift patterns, and the prospect that the worst is still to come.
With the number of Covid cases rising across the capital and the UK, the hospital has vastly expanded intensive care capacity and moved staff without specialist training to high dependency roles to cover the workload.
It comes as a further 1,041 people died within 28 days of testing positive for coronavirus in the UK on Wednesday, the highest daily reported total since the first wave of infection in April.
London has been at the epicentre of the latest wave of infections, and St George's has now seen its number of Covid patients at least matching the first peak.
In rare behind-the-scenes access to a frontline ward, the Press Association was told that staff are "resilient" to the challenge ahead, but workers conceded there was little room for manoeuvre.
Read more: PM to hold press conference as Oxford vaccine rolled out to GPs
Read more: Oxford-AstraZeneca Covid vaccine rolled out to GPs


Dr Mark Haden, an emergency department consultant, said: "We make it look like business as usual but it's very much not - it's very different to our usual pattern of work.
"Everyone's stress levels are higher than usual. Everyone is working to the limit, to the threshold of what they're able to.
"The hospital bed occupancy is very, very high, it has lots of Covid patients as inpatients at the moment. It's very stressful for staff and that is starting to show."
St George's has had to expand the number of intensive care beds for the critically sick from 60 to 120, the vast majority of which are for coronavirus patients.
The rest are for those recovering from other serious trauma such as heart attacks or road traffic accidents.
However, the expansion has had a real impact on both the staff and patients' treatment.
Read more: UK records 62,322 new Covid cases and 1,041 more deaths
Read more: Boris Johnson: UK in final 'sprint' to defeat coronavirus

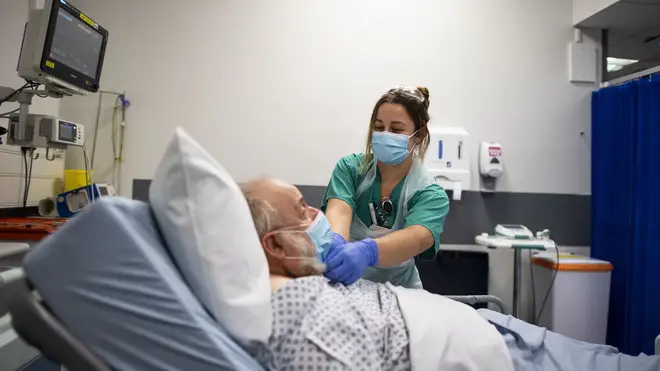
Nurses who would usually be assigned to one patient are now having to deal with up to four casualties at one time.
And they are doing so while wearing uncomfortable personal protective equipment (PPE).
Such is the demand on the intensive care unit that staff from other departments are being drafted in to help - despite not being trained to do so.
ICU consultant Dr Mohamed Ahmed, 40, said: "When a nurse has care of one patient, there's that ratio for a reason - every detail needs to be looked at.
"When they need to look after three or four patients, their standards are lowered.
"They feel they have to do their best but they come away feeling demotivated and demoralised. That's really apparent. They clearly want to do the best they can."

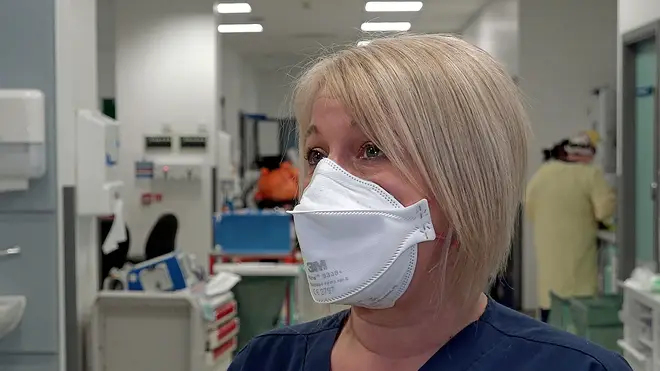
Matron Lindsey Izard said pressures on the service were immense.
"It's not just about Covid," she said.
"If you go up a ladder this weekend and fall off it, there's a chance you won't get an ICU bed.
"People are still getting run over, they're still self-harming, they're still beating each other up."
Ms Izard said staff were so exhausted that she feared "a large number" would quit once the pandemic was over.
She said: "I really do think a lot of people have thought, 'This is the writing on the wall for me as a nurse, I'm not sure I want to do this again'."
It came as an NHS England briefing apparently showed London's hospitals on the verge of being overwhelmed by coronavirus even under the "best case" scenario.
Listen & subscribe: Global Player | Apple Podcasts | Google Podcasts | Spotify